Methods of Diagnosis
Methods of Diagnosis
I have a problem with my pancreas? What tests should I expect?
First of all, on the basis of the symptoms the patient describes to him and a physical examination, the doctor will say that he suspects something is wrong with the pancreas. In order to confirm this suspicion and to establish the exact nature of the pancreatic disorder, a blood test will be carried out, together with one or more additional tests. In the following section, further details are given of the various tests which are available in order to diagnose disorders of the pancreas.
1. The Ultrasound Test (Sonography)
The ultrasound examination is the simplest way of obtaining an image of the inside of the body. Using a form of sensor, which the doctor lays on the skin, sound waves are transmitted into the body.
These waves are reflected by the internal organs and picked up by the same sensor. The strength of the reflected signal varies from organ to organ, and this is used to produce images in which the various internal organs such as the liver, kidneys and pancreas can be recognised. By carefully examining the pictures, the doctor is able to see any changes in the organs which may indicate disease. The test procedure is normally as follows: In order to improve the quality of the image, the patient should not have anything to eat or drink in the 6 to 8 hours before the test (in order to have an empty digestive system), otherwise there will be too much air in the intestines, which will limit the quality of the test. Before the sensor is laid on the body, some jelly will be spread on the skin in order to improve contact between the skin and the sensor. The jelly may feel cold, but otherwise the test procedure does not involve any pain or discomfort. Ultrasound waves have no side effects.

2. Computerised Tomography (CAT Scan)
This is probably the most common procedure used in the diagnosis of pancreatic disorders. The computer tomograph is a form of x-ray machine which produces a large number of cross section images of the body. These give a precise view of the state of the pancreas and the organs surrounding it.
The test procedure is normally as follows: Half an hour or so before the test, the patient has to drink a special liquid (approx. 8 dl of contrast agent). This liquid makes the stomach and intestine appear white in the images and allows them to be easily distinguished from other organs. The test is carried out in a special room and the patient lies on an table which moves automatically. The patient receives instructions and information from the control room by intercom. The CAT machine resembles a wide tube about 1m long, and the patient is moved slowly through it as the cross-section pictures are taken. In the second half of the test another form of contrast agent is injected into a vein in the arm, and this enables blood vessels and internal organs to be seen more clearly. The entire test takes about 30 minutes.
3. Magnet Resonance Imaging (MRI)
The MRI test (Fig. 3) is similar to the CAT test, in that cross-section pictures are again taken. However, the test does not use x-rays, but works using changing magnetic fields. The patient has to lie in an enclosed metal tube and try to remain as still as possible throughout the procedure. Patients who suffer from claustrophobia should inform their doctors before the test is carried out, as should patients who have had a pace-maker fitted or any other prostheses containing metal parts, because, as the test involves the use of magnetism, this could possibly lead to problems. The procedure takes an hour to an hour and a half.

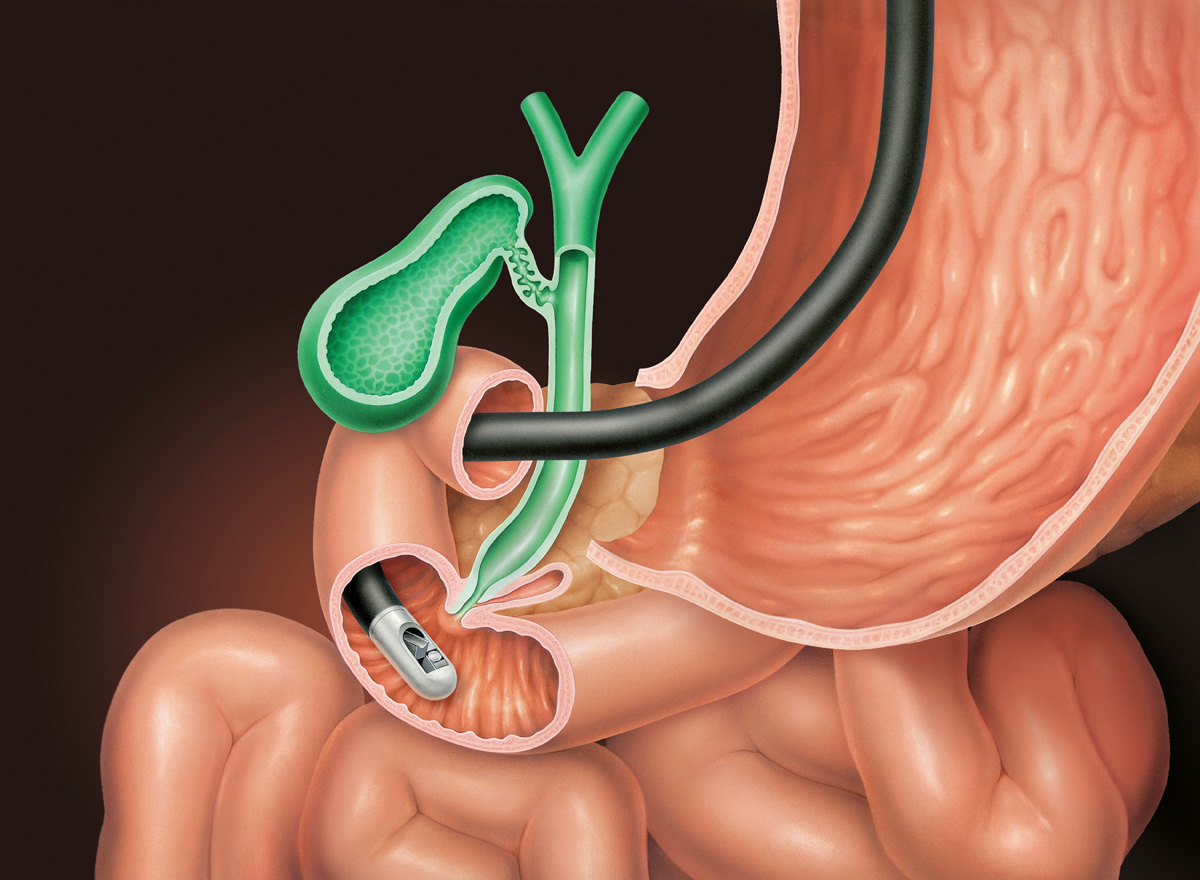
4. Endoscopic Retrograde Cholangio-Pancreatography (ERCP)
ERCP allows a precise examination of the bile ducts and pancreas to be carried out. This is a highly important supplementary test to the other image-producing tests. In the course of ERCP, other procedures can be carried out, such as the removal of a gall stone, which could block the bile duct or the pancreatic duct.
The test procedure is normally as follows: The patient is sedated in order to reduce discomfort during the test. This requires that the patient has nothing to eat or drink in the 6 hours before the test. An intravenous drip is inserted into the forearm, so that the patient can be given a sedative, antibiotics and other medication before and during the test. The patient lies on his side and, as in a gastroscopy, an endoscope is fed into his mouth and through the digestive system until it reaches the duodenum. The doctor follows the progress of the endoscope on a computer screen. When the point is reached where the bile ducts converge with the duodenum, a small tube is fed out of the endoscope and into the bile duct/the pancreatic duct. A contrast agent is now sprayed from the tube into the ducts and x-rays are taken.